Fungal Acne
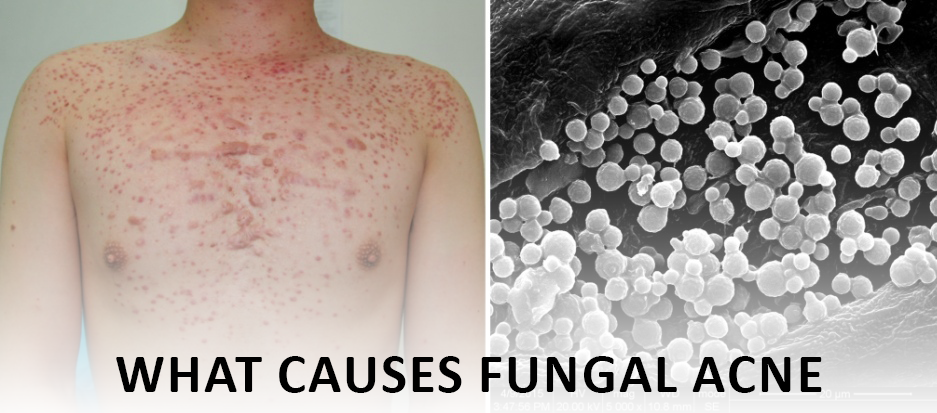
The fungus Malassezia is the cause of Malassezia folliculitis, otherwise known as fungal acne. Acne vulgaris, the standard form of acne, is caused by bacteria. Currently, there are 22 species of this fungus, which is naturally found on our skin. They are opportunistic pathogens. It is harmless, causing disease only when immunity has been compromised somehow. Furthermore, it is also associated with other conditions in dermatology, such as seborrheic dermatitis and dandruff.
For growth, Malassezia needs fat as a food source. Thus, it is commonly found on parts of the body with a dense population of oil-producing glands, such as the scalp, the face, and the trunk. Itchy skin (dandruff) is caused by the rapid fungus growth on the skin. On top of that, the fungus disrupts the natural renewal of skin cells.
How do you know if you have fungal acne?
In some cases, fungal acne can resemble regular acne. As such, it can be challenging to differentiate between the two. Some clues can be found, however. Fungal acne is characterized by red bumps (papules) or pustules (whiteheads) of similar size, rarely larger than 2mm. They sometimes come in waves and can be pretty itchy – much more so than usual acne spots. Fungal acne can occur anywhere on the body, but the following sites are common:
- Forehead and temples
- Upper chest
- Upper and mid-back
Regular acne, on the other hand, has closed comedones (blackheads), open comedones (blue bumps), nodules (red lumps), cysts, and abscesses (spots with pus inside). Locations can also vary in size.
What causes fungal acne?
No one knows for sure what causes fungal acne. Nevertheless, certain conditions can make people more prone to it. Diabetes, HIV, organ transplants and immunodeficiency are a few of these. In addition to obesity and steroid use, studies have linked fungal acne to stress, birth control pills, and birth control pills.
Chronic antibiotic use has also been linked to fungal acne. Antibiotics kill the bacteria that prevent Malassezia from growing on our skin’s surface, altering the delicate balance of microbes. As a result, fungal acne is often misdiagnosed as acne and prescribed antibiotics as soon as possible. The condition is thus further aggravated.
Additionally, some factors influence how quickly the fungus grows. Malassezia multiplies more rapidly in a pH range of 5.5 to 7.5 and humid, hot environments. My experience in Pakistan and the Philippines supports the high incidence of fungal acne in these countries.
Read More: What causes a double chin and How to Get Rid of Double Chin Naturally
Often it is difficult to differentiate between fungal acne and regular acne. We can distinguish the two by looking at a few factors:
- In contrast to acne vulgaris, itching is characteristic of fungal infection rather than acne vulgaris.
- Numerous small, uniform lesions that look like whiteheads. These tend to be more common on oilier parts of the face, such as the forehead.
- Dandruff. As the same fungus can cause both acne and dandruff, people with fungal acne often have dandruff.
How to treat fungal acne?
Choosing the proper skincare is an integral part of treating fungal acne and sticking to it after it has cleared to prevent recurrences. Malassezia is a fast-growing fungus that causes fungal acne, so you need to avoid most oils and a wide range of lipids.
If your acne is severe, it may also be beneficial to use a topical anti-fungal for 3-5 nights once your skincare routine is in order. It may irritate your skin if you leave it on overnight. It is as effective as contact therapy, which involves applying the ointment for 20 minutes and then rinsing it off. You can get 2% ketoconazole ointment from a pharmacist for this purpose. If you cannot find a cream, you can also use ketoconazole shampoo. It can be applied thinly over the affected areas and left on for 10 minutes.
When used in a fungal acne-safe formulation, several active ingredients in skincare can also treat fungal acne and prevent it from recurring. Salicylic acid, which has anti-inflammatory and antibacterial properties and unclogs pores, is an effective ingredient: honey, azelaic acid, sulfur, urea, and even love.
How can you reduce the chance of acquiring fungal acne?
- Avoid hot, humid environments
- Keep clothing loose
- Avoid applying cumbersome layers of cream or makeup to your face
What should I avoid if I have fungal acne?
Fungal acne is a skin condition characterized by red, scaly, and inflamed bumps on the skin. If you have fungal acne, it is important to avoid certain things that can trigger or worsen the condition. Here are some things to avoid if you have fungal acne:
- Moist and humid environments: Fungal acne thrives in warm and humid environments, so avoid staying in such places for long periods.
- Heavy and oily skincare products: Heavy creams, oils, and makeup can clog your pores and create a breeding ground for fungi. Opt for lighter, water-based products instead.
- Synthetic fabrics: Synthetic fabrics, such as polyester and nylon, trap heat and moisture against the skin, which can worsen fungal acne. Wear breathable fabrics like cotton instead.
Conclusion
An infection caused by yeast overgrowth in hair follicles is fungus acne. In spite of its name, it does not cause whiteheads or blackheads like acne. Fungal acne cannot be treated with typical anti-acne treatments. Proper treatment for this type of infection requires accurate identification.